Do you or someone you know have Ulcerative Colitis? Ulcerative Colitis (or UC) is an Inflammatory Bowel Disease that causes ulcers in the digestive tract. While the condition can be frustrating and difficult to manage, it may be possible to continue participating in outdoor activities such as backpacking and hiking with Ulcerative Colitis – albeit with some extra planning and preparation.
Hi, my name is Katy – although on the trail I go by Unicorn. In 2014 I was diagnosed with Ulcerative Colitis. Thankfully, I have a relatively mild form of the disease, but it has still made my life interesting at times. I love to travel, hike long-distance trails and go on adventures – and I’ve been able to do all these things with Ulcerative Colitis. In 2017 I hiked over 1800 miles on the Pacific Crest Trail and had a flare-up in the middle of it.
I this article I’ll share some tips that I’ve learned from my years of backpacking and hiking with Ulcerative Colitis. Keep in mind that that the information presented here is no substitute for advice from your doctor. What works for me may not work for other UC patients, especially ones with a more severe form of the disease. But I hope you find it useful.
Table of Contents
What is Ulcerative Colitis?
Ulcerative Colitis is an autoimmune disease which causes inflammation in the colon and rectum. It’s the same disease as Crohn’s, except Crohn’s Disease persists throughout the entire digestive system. UC, on the other hand, is confined to the colon.
UC and Crohn’s Disease are both forms of Irritable Bowel Disease (IBD). Note that IBD is not the same as Irritable Bowel Syndrome (IBS), even though the symptoms can appear to be similar. IBS is a syndrome that typically does not cause inflammation or hospitalization, whereas IBD is classified as a disease. Patients with severe forms of Irritable Bowel Disease occasionally require hospitalization and surgery.
UC is a chronic disease which means that once a person is diagnosed with it, they have it for life. Sometimes the symptoms go into remission for long periods of time, and sometimes flare-ups occur.
While the disease is usually treatable with medication and diet modifications, unfortunately there is no cure as doctors still don’t fully understand what causes the condition.
My Ulcerative Colitis Diagnosis
I was diagnosed with UC after in 2014 after a vacation to Mexico. When I returned home, I came down with a case of traveler’s diarrhea that never seemed to go away. In fact, the symptoms got progressively worse. When I saw blood in my stool, I began to get worried and contacted my doctor. Several months and a colonoscopy later, I finally had a diagnosis: Ulcerative Colitis.
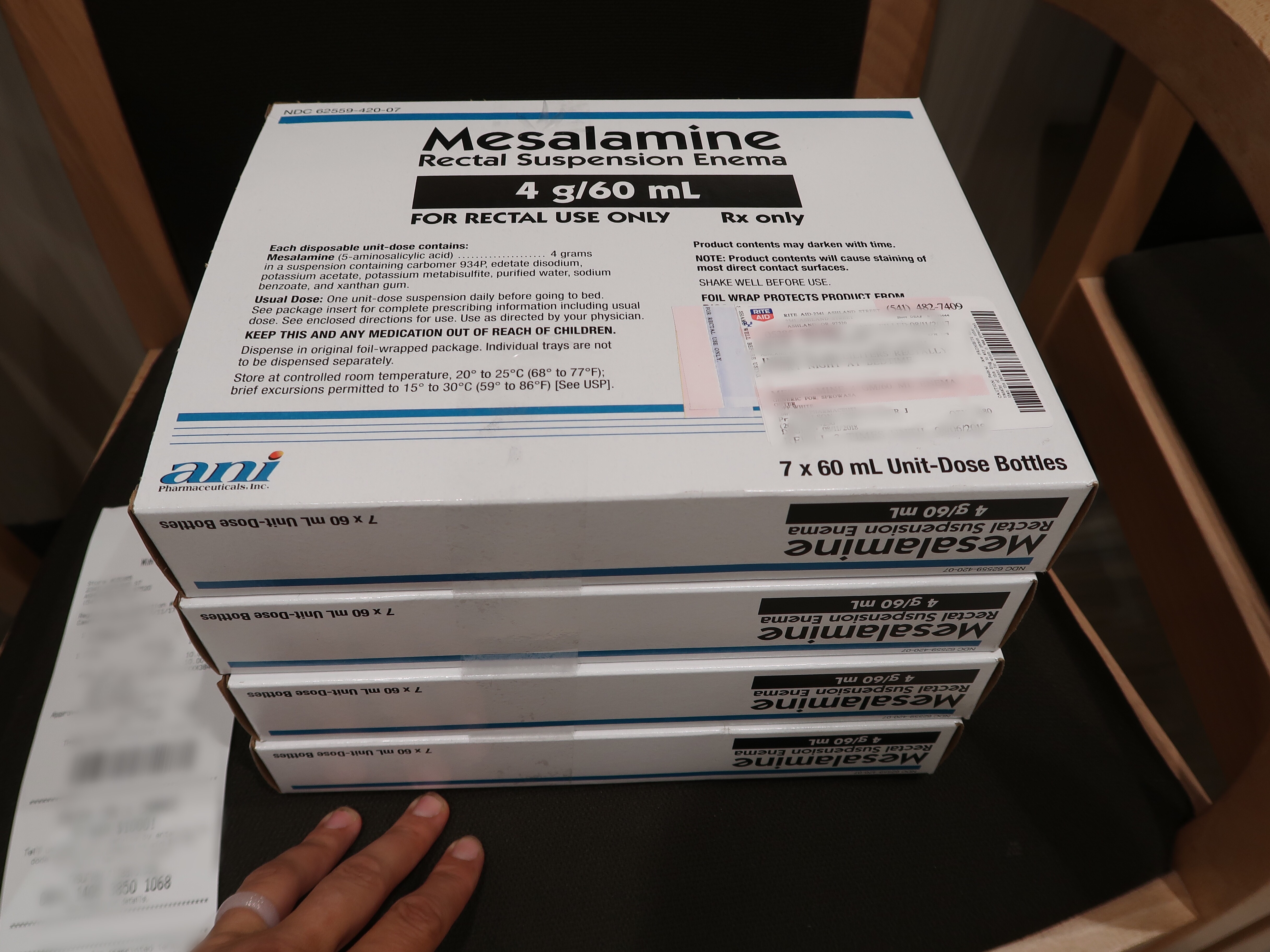
In my case, since the disease is primarily confined to the end of my colon, I take an anti-inflammatory medication called Mesalamine (or Rowasa) that is targeted to the disease’s location. To put it in plainer terms, the medicine is administered via enema every night before I go to bed. It’s not a very pleasant experience but I’ve gotten used to it over the years. I also take Mesalamine pills orally.
While I wasn’t very happy to take enemas when I was first diagnosed, now that I know more about UC I’m grateful to have medicine that treats my disease so effectively. Many people with Ulcerative Colitis are much worse off. Some have to take immune-suppressing drugs or biologics and others must have parts of their colon surgically removed.
My Experience Hiking with Ulcerative Colitis
In 2017, I attempted a thru-hike of the 2600-mile Pacific Crest Trail from Mexico to Canada. At the time, I still was a relatively new Ulcerative Colitis patient and had only experienced one flare-up. In fact, I secretly hoped that it had all been a fluke because I hadn’t had any symptoms in over two years.
After checking with my doctor, I began hiking in April 2017. At first, everything went very well. I traveled over 1000 miles in three months with no complications from my autoimmune disease. I grew stronger and leaner and learned to hike faster.
All that changed in July 2017 when I experienced an Ulcerative Colitis flare-up on trail in the middle of the wilderness. I was miles away from town and didn’t have the right tools to deal with the situation. Suffice it to say that I was miserable to be so far away from a bathroom without running water. And of course I had no enemas stashed in my backpack to treat the disease.
I made a mad dash to Sierra City, the nearest town, and traveled home. After a visit to my gastroenterologist and a battery of tests, my symptoms improved. I was ready to begin hiking with Ulcerative Colitis again…. except this time I had to bring enemas with me to ensure the symptoms did not return.
Long-distance hiking with enemas was a logistical challenge, but it can be done. In order to keep my pack weight as light as possible, I only carried 7 enemas with me on trail at a time. This meant that I had to ship packages of enemas ahead to towns along the trail so I could pick them up at a future date.
I hiked with enemas in my backpack for over 800 miles on the the PCT in 2017 over a span of two months.

Selfie with Dr. Carlson, my gastroenterologist. I paid him a visit when I experienced a Ulcerative Colitis flare-up while hiking the PCT.
Tips on Backpacking and Hiking with Ulcerative Colitis
As previously mentioned, don’t attempt any serious hiking or backpacking adventures without first consulting your doctor. Additionally, I don’t recommend extended wilderness travel if you’re in the middle of a flare-up. Try a shorter hike or a day trip first to get an idea of how serious your symptoms are and what you should bring before attempting a longer trip.
- Always drink filtered water. The last thing you need in the wilderness is to contract giardia or some other nasty bug which could trigger a flare-up. I bring my own potable water or use the Sawyer Squeeze water filtration system for longer backpacking trips.
- Wash or sanitize your hands after using the bathroom. It can be hard to keep clean in the wilderness, but it’s important for UC patients as giardia can be spread from fecal matter. Additionally, avoid touching other hikers’ hands. When sharing food, pour snacks directly into their hands rather than letting people grab directly out of your food bags.
- Bring backup medication. Be prepared in case you start a flare-up in the wilderness and are days away from town. This may not be practical if you are taking biologics which have to be refrigerated (or enemas which are bulky). The next time I hike a long-distance trail, I’ll ask my doctor to prescribe suppositories. These don’t work as well as enemas (for me anyway) but are much lighter and easier to transport. You also may want to bring antibiotics or other medications that are hard to obtain in remote areas.
- Don’t take Ibuprofen. Research has shown that Ibuprofen and NSAIDs such as Motrin, Advil, and Nuprin can can aggravate symptoms and even trigger a flare-up. I was taking a lot of Ibuprofen on the PCT due to a pulled muscle in my foot until my doctor learned about it and told me to stop. In hindsight, I now believe this may have triggered my flare-up on the trail.
- Be prepared to poop in the woods. Bring a small trowel and toilet paper so you can poop in the woods if necessary. To poop in the woods properly, simply dig a cat hole that is 6-8 inches deep and at least 200 feet away from lakes, streams, and hiking trails. Cover the hole with dirt when you are finished and pack out your toilet paper in a Ziploc bag or doggie poo bag. I personally find wet wipes helpful to keep things extra clean (and prevent chafing). If you have an accident, be sure to dig a hole and bury it afterwards. Check out my article on How to Poop and Pee in the woods for more tips.
- Bring extra toilet paper and wet wipes. If you do have a flare-up in the woods, the last thing you’ll want is to do is run out of toilet paper. This happened to me when I hiked the PCT and if it wasn’t for the kindness of friends who shared their toilet paper with me, it would have been a *real* bummer.
- Bring extra underpants. If you start a flare-up in the wilderness, soiling your only pair of underpants isn’t a pleasant experience. Bring an extra pair or two along just in case you accidentally poop your pants.
- Pack out your garbage. This includes used toilet paper, wet wipes, empty enema bottles and soiled underpants. I always bring along a spare gallon-sized Ziploc baggie to store extra garbage in.
- Have health insurance. Be sure to have adequate health insurance so you are covered in case you need to see a doctor, fill a prescription, or worse – go to the hospital.
- Consider bringing a PLB. A Personal Locater Beacon or PLB allows hikers to send a distress call to wilderness search and rescue in areas with no cell reception. I use the Garmin InReach Explorer because it also enables 2-way texting over satellite.
Hiking During a Flare-up
If you are in the middle of a flare-up and have the frequent urge to use the bathroom, I personally wouldn’t recommend starting a long backpacking or wilderness camping trip unless you are an experienced hiker and very familiar with your symptoms. Try a shorter hike or a day hike instead.
- Know where the bathrooms are. Preparation is key when planning an outing during a UC flare-up. If you’re in a front-country setting such as a park or area with other people are around, research where all the bathrooms are and choose a trail that stays close by.
- Be prepared to poop in the woods. This applies for hikes in wilderness settings with no bathrooms and few people around. (See the section above for more details on how to do this properly.)
- Bring extra underpants and a change of clothes. Sometimes accidents happen. No big deal! Just bring a spare pair of underpants. I’ve also been known to wear menstrual pads or other liners on my underpants in case of an accident.
- Drink plenty of water. Diarrhea and frequent bathroom usage can cause dehydration, so be sure to stay hydrated by drinking lots of water.
- Tell your hiking buddies. Let your friends know so they can support you and help locate a bathroom (or quiet place to dig a cat hole) should the need arise quickly.
- Eat foods that won’t aggravate your flare-up. This is different for every person. See the Hiking and Backpacking Food section below for more details.
Hiking/Backpacking Food and Ulcerative Colitis
If you’re wondering what food to eat during a flare-up (or to avoid a flare-up), you’re not alone. There are a lot of web sites and research devoted to this subject with slightly different approaches. Some recommend the Specific Carbohydrate Diet, the Mediterranean Diet, the Low-Residue Diet (aka low fiber diet), the GAPs Diet or a Low-FODMAPs Diet.
The truth is that no single diet works for everyone. That’s why there are so many different ones out there. You should work with a doctor to develop a plan that’s right for you. Doing this properly is a lot of work, as it typically involves closely tracking symptoms and foods to find correlations between the two.
Over the years I’ve tried many approaches to diet such as avoiding gluten, dairy and alcohol. I even consulted a naturopathic doctor once who put me on a strict exclusionary diet. I’ve had mixed success with these diets because it has been really hard to trace a correlation between a dietary change and a symptom.
The one exception to this is the Low-FODMAPs diet. I have been experiencing a lot of bloating and cramping over the past year which has been really uncomfortable. My doctor recommended the Low-FODMAPs diet a few months ago and I noticed an immediate improvement in symptoms.
So, the moral to this story is to keep trying until you find something that works for you.
Additional Resources on Hiking with Ulcerative Colitis
- Crohn’s and Colitis Foundation
Crohn’s and Colitis is a great organization. The web site had a wealth of information for UC patients and should be the first place to start after your diagnosis. - Guide to Hiking and Other Outdoor Activities with UC
This article in Everyday Health has some good advice on hiking with a flare-up or for people who are experiencing a more severe form of the disease. - Crohn’s and Colitis Support Groups
Consider joining a support group. I attended a local support group for a while after my initial diagnosis which was a valuable experience. It’s helpful to remember that you are not alone. - Crohn’s and Colitis Events
Learn more about Ulcerative Colitis and join the IBD community at a Crohn’s and Colitis event. I attended a Crohn’s and Colitis seminar after my initial diagnosis and was glad I did. - Camper Christina – Camping with Colitis
For another perspective on UC, Christina is an avid camper with UC who blogs about her experience.
Like this Blog Post? Pin it!
Note: This post contains affiliate links, which means I may receive a commission if you click a link and purchase something. While clicking these links won’t cost you anything, they will help me to keep this site up and running!








What a great post ! Staying active is really the key to the Universe. You’re an inspiration. I have RA and it has it’s own challenges, but as you say, there is always someone dealing with worse things. Brava ! Looking forward to your coming adventures !
Thanks Bonnie!
Great post. Thank you for including my link and congrats on still getting out there! 🙂 Cheers!
Thanks Christina!
I have UC, and while I’ve only had one real flare (when I got diagnosed), it causes other problems like swollen and painful feet joints. My husband and I are backpacking isle Royale in a few weeks. We’re only going for four days, but I’m pretty nervous about it. Thank you for sharing your experiences!
Hi Kali, thank you for sharing your experience. I haven’t had to deal with swollen and painful feet joints. That sounds awful. Good luck with your backpacking trip!